Barriers to Interprofessional Collaboration
Barriers to interprofessional collaboration in healthcare are one of the main reasons teamwork breaks down and patient care suffers. Imagine a patient with multiple health concerns—a primary care doctor, a nurse, a physical therapist, and a pharmacist all contribute their expertise. Ideally, they would work together smoothly, sharing updates, ideas, and planning care as a unified team. But reality can look very different. Missed messages, conflicting advice, and professional boundaries often stand in the way. So, what stops healthcare professionals from collaborating effectively? Understanding these barriers is the first step toward better teamwork, improved patient-centered care, and safer outcomes for everyone involved.
Why Interprofessional Collaboration Matters in Patient Care
Interprofessional collaboration, often called “team-based care,” brings together professionals from different fields to support patients with comprehensive care. This approach strengthens patient safety, enhances clinical outcomes, and helps healthcare providers make better decisions together. When a care team uses shared decision-making and focuses on continuity of care, the patient receives treatment that considers every aspect of their well-being.
Studies show that collaborative practice reduces medical errors, increases patient satisfaction, and improves job satisfaction among staff. The Institute for Healthcare Improvement reports that hospitals with effective teamwork see fewer readmissions and better quality indicators. However, building successful integrated care teams is easier said than done.

Common Barriers to Interprofessional Collaboration
Barriers to collaboration in healthcare are complex and often interrelated. These obstacles impact everything from daily routines to long-term outcomes.
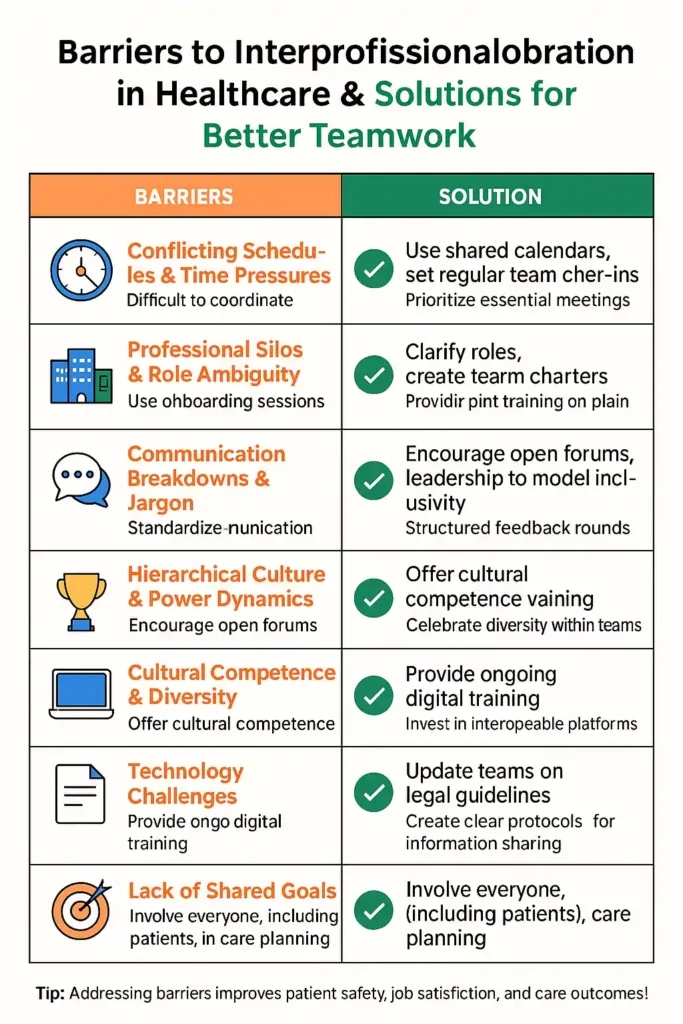
Conflicting Schedules and Time Pressures
Healthcare professionals work in shifts, handle large caseloads, and juggle unpredictable emergencies. Getting everyone together for care conferences or team meetings is challenging. Primary care clinics and hospitals alike struggle to find common times for multidisciplinary discussions. Time limitations often lead to rushed conversations or missed updates, which can impact continuity of care and increase the risk of medical errors.
A study published in the Journal of Interprofessional Care highlights that time pressure is a top complaint across clinical settings, affecting everyone from nurses and speech-language pathologists to surgeons.
Professional Silos and Role Ambiguity
In many organizations, professionals work in silos—sticking closely to their departments and rarely interacting outside their discipline. This separation can lead to fragmented care. Professional identity and rigid scopes of practice sometimes prevent staff from sharing tasks or communicating openly. Role ambiguity makes matters worse: if team members are unclear about responsibilities, important information may fall through the cracks.
For example, a nurse might be unsure about when to escalate a patient’s changing condition, while a pharmacist may hesitate to question a physician’s prescription. These situations create gaps in patient safety and can reduce trust among team members.
Communication Breakdowns and Jargon
Effective teamwork depends on clear communication. Yet, differences in language, terminology, and communication styles often stand in the way. Physicians, nurses, and allied health professionals each have their own jargon, which can cause confusion. Even body language and tone can vary between disciplines, leading to misunderstandings.
For instance, speech-language pathologists working with physicians in a stroke unit may find that clinical updates are rushed or filled with unfamiliar abbreviations. Inconsistent handoffs or incomplete documentation in electronic health records can also result in information gaps that compromise care.
Hierarchical Culture and Power Dynamics
Traditional healthcare environments often operate with strict hierarchies. Senior physicians or administrators may dominate conversations, while junior staff, nurses, or allied health professionals feel hesitant to speak up. These power imbalances can prevent team members from expressing concerns, asking questions, or making suggestions. This issue is especially acute in high-pressure environments like operating rooms or intensive care units.
Hierarchical culture not only limits shared responsibility but also weakens patient-centered care. Junior staff who fear retribution are less likely to point out safety issues or suggest alternative approaches. Addressing these power dynamics is essential for building a collaborative workplace.

Cultural Competence and Diversity
Modern healthcare teams are diverse, with members from various cultural, ethnic, and educational backgrounds. Differences in cultural beliefs, communication styles, and health literacy can affect teamwork. Misunderstandings may occur due to varying expectations for politeness, decision-making, or hierarchy.
Cultural competence—an awareness and respect for diversity—helps teams work together more effectively. Research from the World Health Organization points to the need for training in cultural humility and inclusive communication. Teams that value diversity are more likely to deliver equitable, patient-centered care.
Technology as Both a Barrier and a Tool
Technology, especially electronic health records and telehealth platforms, plays a crucial role in modern care. While digital tools make information sharing easier, they can also create barriers if systems are incompatible or if staff lack adequate training. Some professionals struggle with new software, while others find that excessive notifications or technical glitches interrupt their workflow.
In rural clinics or community health settings, limited access to digital tools can further widen the communication gap. However, when used well, technology can connect integrated care teams across locations, supporting virtual case conferences and real-time documentation.
Legal and Ethical Challenges
Interprofessional collaboration sometimes brings up questions around confidentiality, professional liability, and informed consent. Regulations may limit what can be shared between team members or how information is documented. For example, mental health professionals and medical staff may follow different privacy rules, making it hard to coordinate care for patients with complex needs.
Clear protocols, shared documentation standards, and ongoing training can help teams navigate these legal and ethical considerations. The Institute for Healthcare Improvement offers tools and frameworks to support safe, effective teamwork in compliance with regulations.
Lack of Shared Goals and Patient Involvement
A common problem in healthcare is the lack of clearly defined, shared goals for patient care. Without mutual agreement on priorities, professionals may work at cross purposes, leading to inconsistent treatment plans. Patient-centered care requires that teams involve patients and their families in goal-setting and care decisions.
Engaging patients through shared decision-making helps ensure that all team members are moving in the same direction. This approach supports continuity of care and better health outcomes, particularly for patients with chronic or complex conditions.

Practical Solutions for Overcoming Barriers
It’s possible to break down these barriers with practical, team-driven solutions. Here’s how healthcare organizations can build stronger, more collaborative environments.
Foster a Culture of Respect and Inclusion
Encouraging mutual respect means valuing every team member’s expertise. Leadership should promote a climate where all voices are heard, and input is welcomed from every discipline. Regular team meetings, open forums, and structured feedback sessions help flatten hierarchy and invite participation.
Define Roles and Responsibilities Clearly
Each member of the care team should know their specific role and understand the contributions of others. Role clarity reduces confusion, improves accountability, and supports effective task delegation. Visual aids, checklists, and onboarding sessions can reinforce this understanding.
Improve Communication Skills and Tools
Training programs in active listening, plain language, and assertive communication can reduce misunderstandings. Teams should standardize their use of handoff tools, documentation protocols, and digital messaging platforms to prevent errors.
Technology should support, not hinder, teamwork. Ensure all staff receive training on new systems and that platforms are interoperable across departments. Use visual summaries, care plans, and secure messaging to streamline information sharing.
Invest in Interprofessional Education (IPE)
Bringing professionals together for joint training builds trust and understanding from the start. IPE programs teach teamwork competencies, conflict resolution, and cultural competence. Simulation-based exercises and cross-disciplinary workshops encourage professionals to appreciate each other’s roles.
Organizations can follow frameworks like those from the Interprofessional Education Collaborative (IPEC) to develop teamwork skills and shared values.
Encourage Patient-Centered Care and Shared Decision-Making
Patients and families should have a voice in care planning. Teams that practice shared decision-making see improved satisfaction, better adherence to treatment, and lower rates of hospital readmission. Involve patients early, ask about their goals, and check for understanding at every step.
Regularly Assess and Improve Teamwork
Use collaboration assessment tools and feedback surveys to identify strengths and areas for improvement. Structured team debriefings and regular reviews of care plans can help teams adjust practices as needed. Quality improvement projects focused on communication and collaboration keep everyone moving forward together.
Case Example: Building Collaboration in a Rural Health Clinic
A rural clinic serving older adults faced high staff turnover and inconsistent care. Professionals from nursing, pharmacy, and primary care met only during emergencies. Patients often reported confusion about who was responsible for their care.
The clinic introduced weekly case conferences, role clarification workshops, and cultural competence training. They also updated their electronic health record system to allow shared notes. Over six months, the team saw better communication, improved job satisfaction, and higher patient safety scores.
This example shows how targeted changes, even in resource-limited settings, can bridge gaps and strengthen integrated care teams.
Conclusion
Addressing barriers to interprofessional collaboration in healthcare is crucial for building strong teams and delivering safe, effective patient care. When organizations recognize these obstacles—whether they’re related to communication, roles, culture, or technology—they can take practical steps to foster better teamwork. Prioritizing clear communication, mutual respect, and patient-centered care helps break down walls between professionals and creates an environment where everyone can contribute fully. As healthcare continues to evolve, overcoming these barriers will remain key to achieving better outcomes for both providers and patients.