Barriers to Communication in Healthcare
Have you ever left a doctor’s office feeling confused or unheard? Or noticed a medical team scramble because something got lost in translation? Barriers to communication in healthcare are more common than most people realize, and they can affect everything from patient safety to staff morale.
These barriers aren’t just about language. They include health literacy, technology hiccups, cultural differences, emotional hurdles, and system-level obstacles. When communication breaks down, the results can be serious—missed diagnoses, medication mistakes, or patients not following important instructions.
So, what exactly gets in the way of great communication in healthcare, and how can medical teams, patients, and families break through? Let’s uncover the biggest hurdles and find practical solutions together.
Understanding the Key Barriers to Communication in Healthcare
Good communication is the backbone of safe, high-quality healthcare. But it’s not always easy to achieve, especially with so many moving parts in hospitals, clinics, and even virtual appointments. Here are the major barriers you’ll find in real healthcare settings.

Language and Interpreter Barriers
It’s hard to overstate how important clear language is in medicine. In the U.S., about 1 in 5 people speak a language other than English at home. Many patients need instructions, diagnoses, and prescriptions explained in their first language. Without trained medical interpreters, mistakes happen—sometimes with life-changing consequences.
It’s not just spoken language. Medical terminology can sound like a foreign language even to native speakers. Imagine being told, “You have hypertension and need an echocardiogram,” instead of “Your blood pressure is high and we’ll do a special heart scan.” That gap is a communication barrier in itself.
Tip: Hospitals and clinics should always provide access to certified medical interpreters, not just bilingual staff or family members. CDC’s Health Literacy page offers resources for improving patient understanding.
Health Literacy
Health literacy means how well someone can understand and use health information. Shockingly, only about 12% of U.S. adults are considered “health literate” according to Healthy People 2030. This gap can lead to patients misunderstanding instructions about medications, follow-ups, or even when to call for help.
Patients with low health literacy might nod along but not truly grasp what’s being said. They may struggle with forms, medication labels, or insurance documents. Even highly educated people can have low health literacy if they’re under stress, facing a new diagnosis, or just overwhelmed.
Tip: Use the “teach-back” method. After explaining, ask the patient to repeat the information in their own words to confirm understanding.
Cultural Differences and Bias
Culture shapes how people talk about health, pain, family, and even death. Some cultures may expect direct communication, while others find it rude. In some communities, it’s common for family to make decisions, while others prioritize patient autonomy.
Cultural misunderstandings can lead to mistrust, refusal of care, or confusion. Bias—whether conscious or unconscious—can also get in the way. Providers must be aware of their own assumptions and stay open-minded when caring for people from diverse backgrounds.
Tip: Invest in cultural competence training and always ask about a patient’s preferences, beliefs, and values.
Emotional and Psychological Barriers
Fear, anxiety, shame, or past trauma can keep patients from asking questions or sharing symptoms. Imagine a teenager too embarrassed to admit substance use or an older adult afraid to discuss memory loss. Providers, too, may avoid tough topics out of discomfort or time pressure.
Patients facing a new diagnosis may feel overwhelmed, leading to poor recall of instructions. Mistrust—sometimes due to prior negative experiences—may make some patients less likely to share important details.
Tip: Build rapport by listening actively, showing empathy, and creating a judgment-free space for discussion.
Barriers for People with Disabilities
Not every patient communicates in the same way. Deaf or hard-of-hearing patients need sign language interpreters or written materials. Blind or visually impaired patients may need braille, audio instructions, or screen readers. Patients with speech or cognitive disabilities (such as after a stroke or living with autism) might use communication boards or other assistive technology.
Physical environments can be a barrier too—think of noisy waiting rooms or inaccessible forms.
Tip: Healthcare providers must ensure accessibility—both physical and digital—so every patient can express themselves and understand their care.
Technology Gaps and Digital Communication
Telehealth, patient portals, and electronic health records (EHRs) can improve communication—but only if everyone can use them. Some patients lack access to reliable internet, devices, or the digital skills needed for online appointments or e-messages. Even staff may struggle with new technology or EHR systems.
Digital communication can be less personal, making it harder to catch non-verbal cues or build trust.
Tip: Offer digital literacy support and alternatives (like phone calls or in-person visits) for patients who need them. AHRQ’s TeamSTEPPS offers tools for improving communication among healthcare teams, including using technology effectively.
Interprofessional and Team Communication Barriers
Healthcare is a team sport—doctors, nurses, pharmacists, therapists, and support staff all play a role. When information doesn’t flow smoothly between team members, mistakes happen. This might mean a medication order is misunderstood, a lab result is missed, or discharge instructions aren’t updated.
Shift changes, handoffs, and unclear protocols can all cause breakdowns. Tools like SBAR (Situation-Background-Assessment-Recommendation) can standardize team communication, but require training and practice.
Tip: Regular team huddles, clear handoff protocols, and a culture of speaking up all help reduce these barriers.
Privacy, Confidentiality, and Trust
Patients may worry about who sees their medical information, especially with sensitive topics like mental health or reproductive care. Strict privacy laws are essential, but confusion or fear about confidentiality can prevent patients from sharing important information.
Sometimes, overzealous privacy measures can block needed information sharing within care teams.
Tip: Providers should explain how patient information is protected and clarify who will have access. Open conversations about privacy can build trust.
Organizational and Systemic Barriers
Time pressure, staffing shortages, rushed appointments, and administrative red tape can all squeeze out good communication. When doctors and nurses are overwhelmed, they may skip thorough explanations, use too much jargon, or not check for understanding.
Lack of standardized procedures or leadership support can mean best practices fall by the wayside.
Tip: Healthcare leaders should invest in ongoing staff training, standardize protocols, and protect time for meaningful patient conversations.
Socioeconomic Barriers and Social Determinants
Communication is affected by issues like cost, lack of insurance, transportation problems, or housing instability. If a patient is worried about paying for care or missing work, they may not fully process or act on health advice. Social workers and patient navigators can help bridge these gaps.
Tip: Ask patients about barriers to care and connect them with support services as part of routine care.
How Technology Is Changing Communication in Healthcare
Technology can break down barriers—but only if used wisely. Electronic health records let teams share information instantly, but only if systems are compatible. Patient portals empower patients to check results, ask questions, and schedule appointments.
Telemedicine increases access but can be hard for those without internet, devices, or digital skills. Language translation apps and captioning tools are improving, but human interpreters are still essential for medical conversations.
Tip: Blend technology with a personal touch. Always check patient comfort and accessibility before relying on digital tools.
Practical Solutions for Overcoming Barriers to Communication in Healthcare
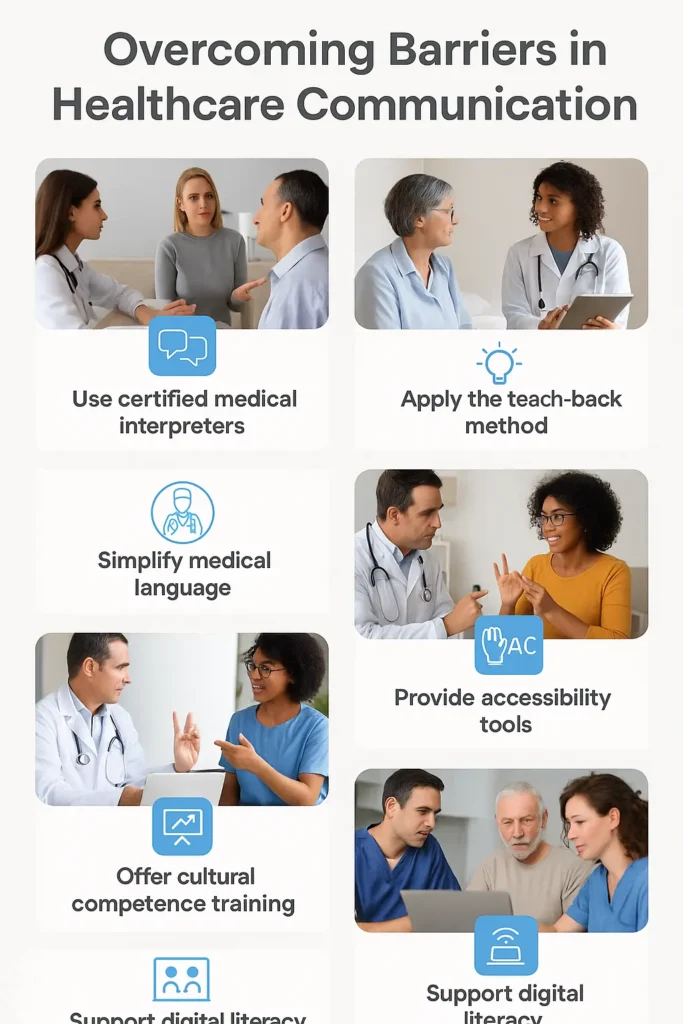
- Use plain language: Avoid jargon. Explain medical terms simply.
- Teach-back method: Ask patients to repeat information to confirm understanding.
- Certified interpreters: Never rely on family or untrained staff for important conversations.
- Cultural competence training: Help staff recognize and respect cultural differences.
- Accessibility: Provide sign language, braille, large print, or digital tools as needed.
- Standardize communication: Use SBAR and checklists for team handoffs.
- Address health literacy: Use written, verbal, and visual materials at a fifth-grade reading level.
- Encourage questions: Create a welcoming environment for patient and team input.
- Build rapport: Listen actively, make eye contact, and acknowledge patient emotions.
- Leverage technology wisely: Combine digital and face-to-face communication based on patient needs.
Real-World Example
A Spanish-speaking patient arrived in the ER with chest pain. The triage nurse used a certified medical interpreter, not a family member, to gather a history. Thanks to clear communication, the team discovered a medication allergy that would have been missed. The patient received the right treatment—and left the hospital safe and grateful.
This scenario highlights how breaking down language and health literacy barriers can have life-saving results.
Conclusion
Barriers to communication in healthcare are everywhere—from language and technology to stress, time, and culture. But with the right strategies, every healthcare provider and patient can be part of the solution. Simple habits—using plain language, listening carefully, involving interpreters, and respecting patient backgrounds—make a world of difference.
Remember, effective communication is the foundation of safe, compassionate, and high-quality healthcare. By tackling these barriers together, we help every patient feel heard, valued, and well-cared-for. Want to know more? Check out our other resources on improving health literacy and building strong patient-provider relationships.




