Barriers of Communication in Nursing
In the bustling world of healthcare, effective communication between nurses and patients is pivotal. But what happens when this vital link faces obstacles? Recent studies have unearthed some intriguing insights into this issue.
A significant study conducted at two hospitals affiliated with Alborz University of Medical Sciences delved into the barriers that hinder nurse-patient interactions. The findings? A shortage of nurses, work overload, and insufficient time for patient interaction emerged as significant impediments. Interestingly, these factors echo in various other global studies, underscoring their universal impact on healthcare communication.
As we navigate the complexities of nurse-patient communication, it’s essential to understand these barriers and their implications. So, let’s dive deeper into these challenges and explore potential solutions to enhance the quality of care.
Understanding the Barriers of Communication in Nursing

Building on our previous discussion about the universal aspects of barriers in nurse-patient interactions, let’s delve further into language proficiency and communication, environmental factors, and disease-specific challenges that contribute to communication difficulties. Understanding these will guide us towards crafting strategies to overcome these communication barriers.
The Importance of Effective Communication in Nursing
Cognition of disease conditions is imperative for healthcare professionals, but it’s equally crucial for these professionals to communicate patients’ oral and written medical information accurately and effectively. For instance, nurses, being the bridge between patients and the extended care team, shoulder a profound onus of communication in healthcare.
Nurses’ clinical acumen, coupled with their communication skills, lays the foundation for a strong nurse-patient relationship. Communication aids are often key to unlocking comprehensive healthcare, guiding patients through their disease conditions, investigators in medical facilities, and other healthcare professionals involved in patient care.
Cultural sensitivity in healthcare can’t be overstated. Healthcare professionals, especially nurses, interact with diverse cultural groups, often encountering language barriers. Language interpreters, despite their viability, are not always available. Such constraints magnify the necessity for enhancing language proficiency and adopting adaptive communication methods in nursing.
Environmental factors also play a significant role in influencing communication. For example, a noisy surrounding might deter effective interaction, while a calm and peaceful space might promote it.
Disease-specific communication challenges present yet another aspect. The complexity of a disease condition often demands a tailored communication approach. A clear understanding of these challenges can spur nurse training in communication skills custom-made to suit such scenarios.
Lastly, educating patients on effective communication is another avenue to explore for overcoming communication barriers. An informed patient might help create a conducive communication environment, further fortifying the nurse-patient relationship.
Understanding these barriers and improving cultural competency, enhancing language proficiency, creating conducive communication environments, and adapting communication methods are critical steps towards overcoming communication barriers in nursing. With the right blend of training and techniques, we can navigate these barriers and achieve effective communication in nursing, benefiting patient care and outcomes.
Common Barriers to Communication in Nursing
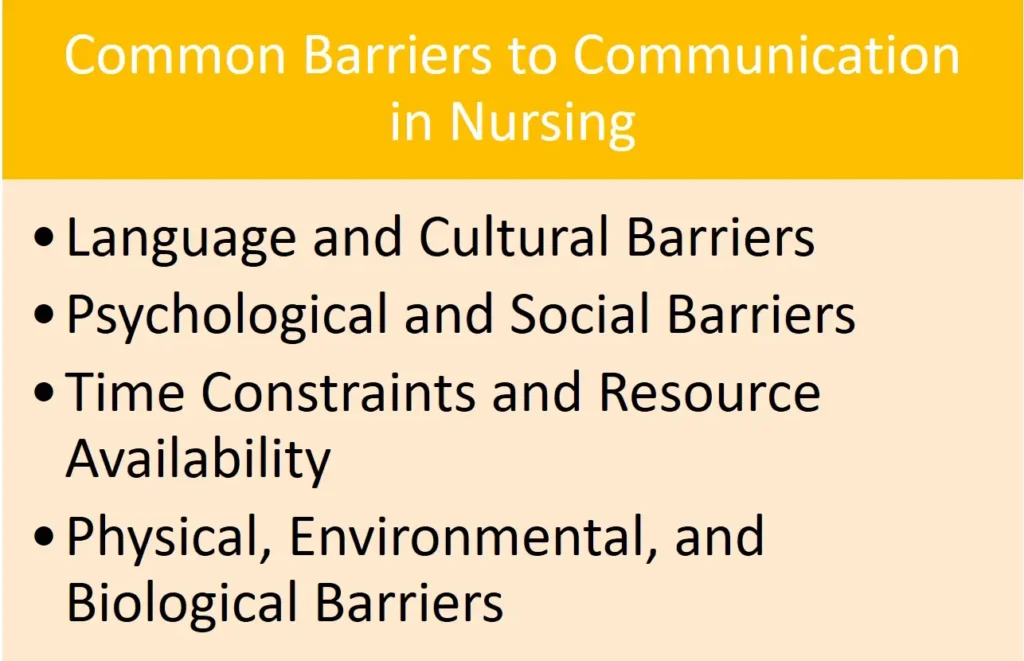
The delivery of quality healthcare depends largely on the robustness of communication among nurses and patients. Diverse barriers exist within the medical facilities which can impede this critical aspect of healthcare. As a professional with substantial experience, I’ll discuss below some of these critical barriers and the impact they have on the nurse-patient relationship.
Language and Cultural Barriers
Language proficiency greatly affects the communication process. Nurses often encounter patients who speak different languages, resulting in a communication gap. Consequently, the lack of understanding negatively affects both parties. Language interpreters are sometimes employed, but even this remedy might not completely resolve the issue due to the intricacies involved in medical communication. Cultural differences also contribute to miscommunication. Nurses must interact with patients from different cultural groups. The absence of cultural sensitivity in healthcare may lead to misinterpretation of messages, thus hindering effective healthcare delivery.
Psychological and Social Barriers
The psychological state of both patients and healthcare professionals plays a significant role in communication. Patients may withhold information due to embarrassment, fear, or discomfort, thereby preventing nurses from comprehensively understanding their disease conditions. Similarly, the excessive workload and stress experienced by nurses can affect their mental state, consequently impairing their communication and empathy skills.
Time Constraints and Resource Availability
Undoubtedly, adequate time is vital to conduct thorough conversations with patients. However, the high workload and fast-paced environment in healthcare do not always allow for such interactions. As a result, communication is sometimes rushed and critical information may be overlooked.
Physical, Environmental, and Biological Barriers
Lastly, physical barriers such as hearing, visual, or speech impairments also pose substantial challenges to communication. Medical facilities must therefore, provide necessary communication aids to ensure information between the parties is effectively relayed. Similarly, environmental factors, like noise and privacy issues, can negatively impact communication efforts.
Improving nurses’ training in communication skills, enhancing their language proficiency, and creating a conducive environment for communication can help overcome these barriers. Additionally, educating patients on effective communication strategies can bridge the communication gap and foster a healthier nurse-patient relationship. It’s crucial that healthcare takes these factors into account to ensure streamlined communication, ultimately improving patient outcomes.
Communication between Nurse Practitioners and Physicians
Building on our understanding of communication obstacles in nursing, let’s explore barriers between nurses and physicians. The most significant obstacle here comes from long-standing hierarchical relationships. Though healthcare has moved towards interdisciplinary teams, historical notion positions physicians as primary decision-makers, influencing communication.
Two main barriers here are psychosocial and organizational. Psychosocial barriers stem from stereotyping, bias, or preconceived ideas about roles and responsibilities. For instance, a physician might bypass a nurse’s view due to bias, or a nurse may refrain from expressing their viewpoint over reputation concerns.
Organizational barriers spring from the dynamic and intense nature of healthcare settings. Factors like heavy workload, shift rotations, and time pressure can limit direct communication between nurses and physicians. Furthermore, an absence of communication protocols or established routes for raising concerns can stifle productive dialogue.
Addressing these barriers means training healthcare professionals in effective communication skills, promoting cultural sensitivity in healthcare, and adapting communication methods to suit changing disease conditions and diverse patient groups. We’re fostering a richer nurse-patient relationship and cultivating a more conducive communication environment in medical facilities. By doing these, we are not just improving the nurse-practitioner-physician communication, but also enhancing the quality of patient care.
Consequence of Communication Barriers on Patient-Centered Care
Communication barriers in the healthcare environment, particularly between nurses and patients, can lead to multiple adversities hindering effective patient-centered care. Two prime areas of impact include the quality of nursing care and patient satisfaction and safety.
Impact on Quality of Nursing Care
When communication between patients and healthcare professionals, especially nurses, becomes obstructed it directly affects the quality of care provided. Take language proficiency, for example. Both nurses and patients need to clearly comprehend each other’s dialogues to administer and receive appropriate care.
Difficulties in understanding language, coupled with possible discrepancies in cultural sensitivity, might result in incomplete or misleading information transfers, hampering effective treatment efforts. Similarly, environmental factors in medical facilities, like the hospital culture or differing power dynamics in nurse-physician relationships, could interfere with open, constructive dialogues necessary for superior nursing care.
Moreover, disease-specific communication challenges might also compromise the quality of care. For instance, a patient with a cognitive disorder might struggle to convey their symptoms accurately, and a nurse may find it challenging to elicit necessary information.
Training nurses in communication skills and enhancing their cultural competency can help assuage these difficulties to some extent. Adapting unique, patient-oriented communication methods and using communication aids may further facilitate in creating conducive communication environments and crafting a more personalized, effective nursing care plan.
Implication on Patient Satisfaction and Safety
Communication barriers not only impinge on the quality of nursing care but also have a profound impact on patient satisfaction and safety.
Patients like being heard, understood, and respected in medical interactions. When a nurse listens actively, responds empathetically, and communicates effectively, it fosters a trusting nurse-patient relationship. Language barriers, lack of cultural sensitivity, or inadequate communication skills may disrupt this relationship.
Nurses, being the key contact point for patients in healthcare settings, play a significant role in patient satisfaction. Patients who experience trouble in communicating their disease conditions, feedback, or queries may get frustrated, leading to reduced satisfaction levels.
Patient safety is yet another area to which communication barriers pose a risk. Miscommunications may contribute to medical errors, creating potential hazards to patient safety. Addressing these barriers by educating patients on effective communication and fostering a culture of robust communication among healthcare professionals is paramount for maintaining patient satisfaction and ensuring safety.
Practical Strategies to Overcome Communication Barriers in Nursing
The solutions here aim to bolster nurse-patient as well as inter-professional relationships through improved communication. As part of my research, I’ve segmented the approaches into three categories that I’ll outline below.
Promoting Person-Centered Communication
Begin by emphasizing person-centered communication, a powerful tool that can cut through barriers in nursing. This approach, put simply, involves engaging patients and their families actively in making decisions about their care requirements. It fosters a stronger nurse-patient relationship while enhancing the overall treatment outcomes.
For instance, by valuing a patient’s dignity and rights and inviting them to negotiate care procedures, the communication becomes more transparent and collaborative. Shared amongst providers, patients, and their families, this type of communication boosts care provision {1}. Therefore, integrating person-centered communication within nursing practices will considerably improve patient-centered care.
Task and Process-Centered Communication Approaches
Equally crucial are task and process-centered communication approaches. Healthcare professionals, particularly nurses who often act as the communication link, must prioritize delivering clear, concise, and complete information. An effective method to achieve this is the patient teach-back strategy {2} which encourages patients to repeat the information to confirm understanding and adherence to care instructions.
Another example of task-centered communication is using communication aids for patients with language proficiency issue. These aids might include visual tools such as pictures and diagrams, written words or translations using language interpreters. This proactive approach of adapting communication methods significantly improves the quality of healthcare provided even with barriers like language and cultural differences.
Advanced Training for Better Communication Skills in Nursing
Lastly, advanced training for improving communication skills in nursing is indispensable. This could encompass a variety of actions, from enhancing language proficiency to heightening cultural competency and broadening disease-specific communication capabilities. By supplementing language skills, nurses can break down the language barriers, allowing better exchange of information and mutual understanding between patients and healthcare professionals.
Training in cultural sensitivity, on the other hand, can equip nurses to effectively communicate across multicultural settings. By understanding and respecting varied cultural groups, it’s possible to customize patient education and improve nurse-patient engagement {2}.
On top of these, special training dealing with disease-specific communication challenges and environmental aspects affecting communications can go a long way in ensuring effective nurse-patient communication. For instance, a nurse dealing with dementia patients can be taught special skills to communicate effectively with such patients {3}.
Promoting person-centered communication, implementing task and process-centered communication methods, and providing advanced training in communication skills can all play instrumental roles in overcoming communication barriers among nursing professionals.
Conclusion
Breaking down barriers in nursing communication is no small feat, but it’s crucial for patient-centered care. By recognizing the challenges, such as language proficiency and cultural differences, we’re already on the path to improvement. Training in communication skills and cultural sensitivity can bridge the gap between nurses and physicians. Practical strategies like person-centered communication and task-process centered approaches are valuable tools in overcoming these hurdles. With advanced training and these strategies, we can enhance nurse-patient relationships and improve treatment outcomes. It’s clear that fostering effective communication in healthcare is a worthy pursuit, ensuring not only better patient outcomes but also a more harmonious healthcare environment.




