Sensory Barriers to Communication
Imagine trying to talk to someone at a busy train station. The noise, flickering lights, and constant movement can make it almost impossible to understand each other. For many, these hurdles are rare and temporary. For others, especially those with sensory impairments, this is daily life. Sensory barriers can disrupt more than just a chat—they can affect access to education, healthcare, and meaningful relationships.
So, what exactly are sensory barriers, and why do they matter so much? This post breaks down the different types, explains who faces them, and shares practical solutions for building more inclusive spaces where everyone can connect.
Sensory barriers are just one of many barriers to effective communication that people encounter in daily life.
What Are Sensory Barriers to Communication?
Sensory barriers occur when someone’s ability to see, hear, process, or interpret information through their senses is different from what most expect. These obstacles can make exchanging ideas, instructions, or emotions tough. They appear in classrooms, medical centers, offices, and public spaces. The Centers for Disease Control and Prevention (CDC) reports that over 11 million Americans are blind or visually impaired, and nearly 16% of adults have some hearing loss [CDC – Disability and Health Data].
Communication relies on more than words—it involves tone, facial expressions, body language, and cues in the environment. When a sense like hearing, vision, touch, smell, or taste works differently, the entire process changes. Barriers don’t just affect the individual; they impact families, colleagues, and communities trying to share messages or provide support.
Types of Sensory Barriers
Most people think of sensory barriers as hearing loss or blindness, but they include so much more. Let’s look at several types and how each can shape communication:
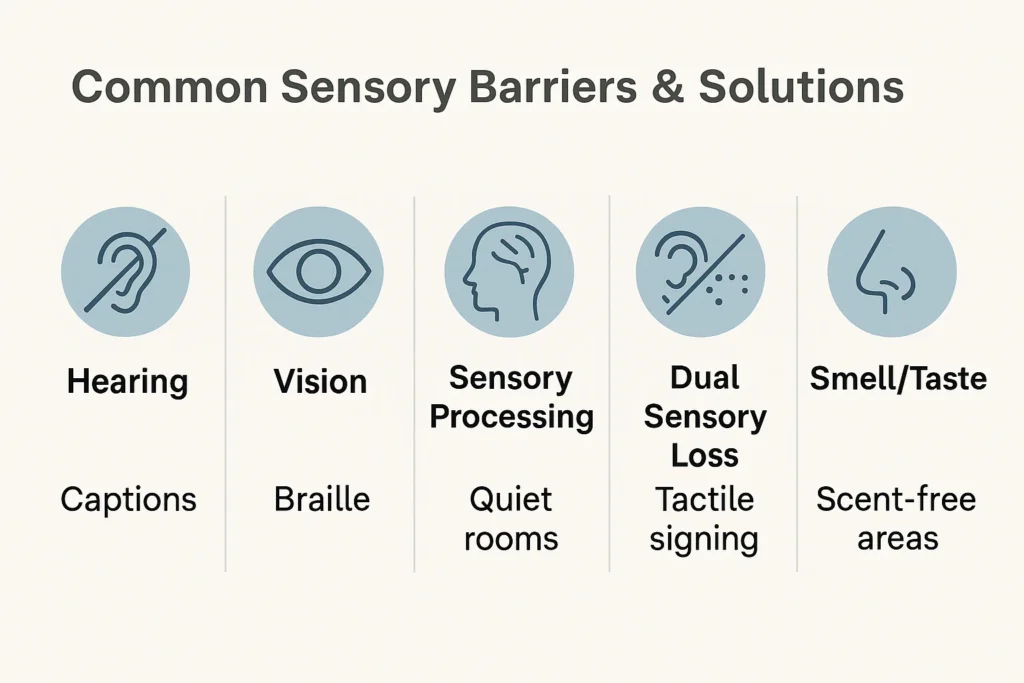
Hearing Barriers
People with hearing loss can find it tough to join group conversations, hear emergency alerts, or catch subtle changes in tone. Even mild impairment makes noisy places stressful. Assistive listening devices, real-time captioning, and sign language are all helpful.
For instance, hearing loops and captioned telephones help users catch important details at work and home. Organizations such as the National Deaf Center provide resources for schools and employers.
Vision Barriers
Vision loss makes reading text, spotting gestures, or following presentations tricky. Poor lighting or cluttered signs cause confusion and anxiety, particularly in new settings. Braille, large print, audio instructions, and tactile maps offer alternative ways to share information.
The American Foundation for the Blind suggests improvements like high-contrast signs, audio cues in elevators, and digital accessibility tools to support users with vision impairments.
Sensory Processing Barriers
Some individuals, especially those with autism or sensory processing disorder, struggle with overwhelming sights, sounds, or touch. Flickering lights, background noise, or unexpected physical contact can make focusing difficult.
Noise-canceling headphones, predictable routines, and calm zones create safer environments for those with sensory processing challenges. Healthcare providers and educators increasingly use sensory-friendly rooms to reduce stress and anxiety.
Dual Sensory Loss and Other Barriers
People living with both hearing and vision loss, known as dual sensory loss or deafblindness, require unique communication tools. Tactile signing, braille technology, and haptic feedback open new channels.
Don’t forget olfactory and gustatory barriers—some cannot tolerate strong smells or certain tastes, which may complicate dining, healthcare, or even social interaction.
Legal Rights and Accessibility Standards
Every person deserves equal access to information, services, and opportunities. Laws like the Americans with Disabilities Act (ADA) in the United States require public spaces, schools, and employers to remove obstacles and provide reasonable accommodations.
Internationally, the United Nations Convention on the Rights of Persons with Disabilities (UNCRPD) sets guidelines for countries to make societies more inclusive. These standards encourage universal design, meaning spaces, products, and technologies should be usable by everyone—no matter their sensory abilities.
Employers and educators need to know their legal responsibilities. Failing to provide access isn’t just unfair—it can be against the law. Providing reasonable adjustments, such as text-to-speech software or accessible signage, is both ethical and necessary.
Assistive Technology
Advances in technology offer powerful ways to overcome sensory barriers. Text-to-speech programs, real-time transcription apps, hearing loops, and screen readers give users flexible options for connecting.
For example, apps like Live Transcribe, Ava, and Otter help turn spoken words into text instantly. Braille displays and screen magnifiers convert digital content for users with vision loss. Many workplaces now offer accessible teleconferencing with built-in captions and adjustable font sizes.
Smartphones, smart home devices, and wearable tech also boost independence. Tools like Be My Eyes connect visually impaired users to sighted volunteers for on-demand visual support.
Environmental Design for Sensory Accessibility
Designing spaces with sensory needs in mind makes a huge difference. Universal design means considering everyone from the start—not just adding fixes later.
Think about lighting. Avoid harsh fluorescent bulbs and use adjustable lamps. Color contrast on signs and walls helps people with low vision. For hearing accessibility, acoustic panels absorb noise and hearing loop systems connect to hearing aids.
Calm rooms or “quiet zones” in schools, hospitals, and airports give people a place to recharge. Tactile pathways and braille maps make navigation smoother. Simple adjustments, like clear signs or textured flooring, improve safety for everyone.
Digital spaces also need attention. Websites should use alt text, high contrast, keyboard navigation, and video captions. The Web Content Accessibility Guidelines (WCAG) outline how digital content can be made accessible to users with different needs.
Addressing Social Attitudes and Stigma
Technology and design are only part of the solution. Attitudes and social awareness matter just as much. Misunderstandings or assumptions about sensory impairments can make people feel excluded.
Disability awareness training for staff, open conversations about accommodations, and listening to feedback all help build trust. Encouraging empathy and patience supports more welcoming workplaces and communities.
Language is important too. Using person-first language—like “a person with hearing loss”—shows respect. Promoting inclusive communication benefits everyone, not just those with disabilities.
Digital Communication
More people now work, study, and socialize online. This shift has brought new accessibility challenges. Videos without captions, poorly contrasted websites, and lack of keyboard shortcuts all limit participation.
Simple steps can make online spaces more inclusive. Always provide captions on videos. Use headings and lists so screen readers work better. Offer transcripts for audio content. Clear navigation and easy-to-read fonts benefit all users—not just those with sensory barriers.
Employers and educators should choose digital tools with strong accessibility features. For example, video conferencing apps with live captioning help participants follow meetings. Email platforms that support screen readers allow everyone to stay informed.
Intersecting Barriers: Sensory Challenges and Diversity
Sensory barriers don’t exist in a vacuum. They intersect with other factors, like age, culture, language, and additional disabilities. For example, older adults may develop hearing or vision loss as they age, while non-native speakers with sensory impairments face double challenges.
Cultural differences can shape how people seek help or express their needs. Organizations should consider diversity when creating policies and programs, ensuring support is truly inclusive.
Early detection and assessment make a real difference. Regular hearing and vision screenings, especially for children and seniors, help identify needs before they grow into larger issues. Schools, clinics, and community centers play key roles in providing resources and referrals.
Community, Family, and Peer Support
Overcoming sensory barriers is rarely a solo journey. Family members, friends, caregivers, and support groups all play essential roles. Encouragement, patience, and shared learning help people adapt and thrive.
Peer networks—both in person and online—offer a safe space to swap tips, share struggles, and celebrate successes. Local advocacy organizations often host workshops, support groups, and social events. Connecting with others who “get it” can make daily challenges easier to handle.
Caregivers, teachers, and employers should listen to people with sensory impairments and incorporate their feedback into programs and practices. Tailoring strategies to individual needs leads to better outcomes for everyone.
Practical Solutions and Tools for Everyday Life
Here’s a quick toolbox for breaking down sensory barriers in real-world situations:
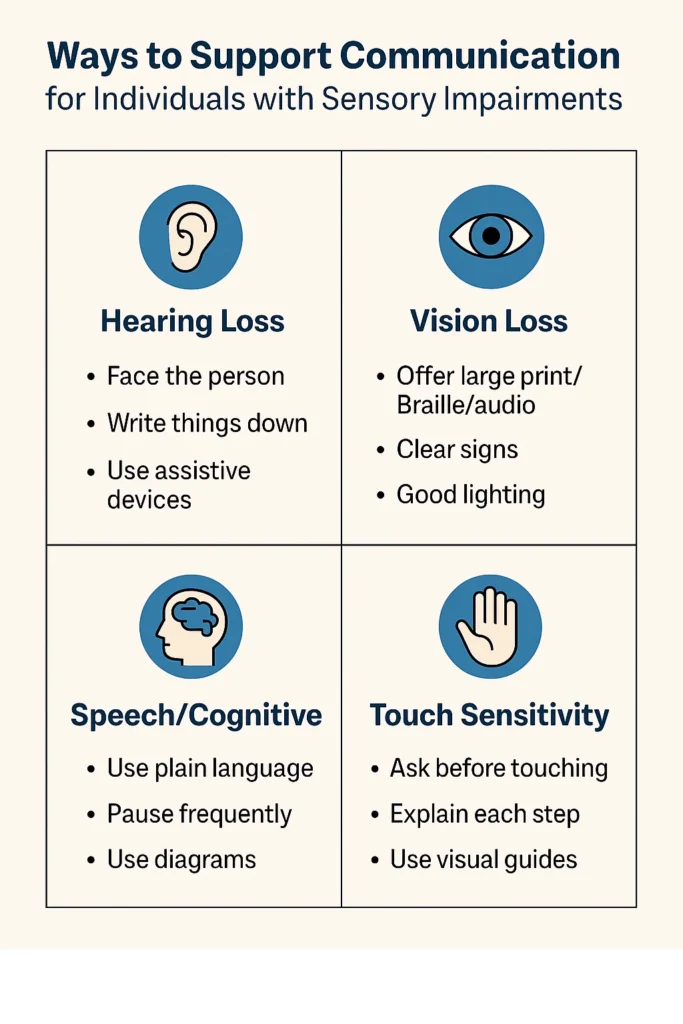
- Clear speech: Face the listener, speak naturally, and use gestures.
- Visual aids: Use diagrams, written notes, and large-print materials.
- Accessible technology: Offer screen readers, hearing loops, or real-time transcription apps.
- Universal design: Include tactile pathways, braille signage, and color-contrast markings.
- Environmental modifications: Create quiet rooms, use soft lighting, and limit background noise.
- Communication alternatives: Learn basic sign language or offer picture-based instructions.
- Feedback: Regularly ask for input from people with sensory needs.
When choosing tools or making changes, check for reputable resources and certifications, such as the International Association of Accessibility Professionals (IAAP).
| Sensory Barrier | Support Strategies |
|---|---|
| Hearing Loss | Face the person, write key points, use assistive tech |
| Vision Loss | Provide large print/Braille/audio, clear lighting |
| Sensory Processing | Offer quiet spaces, predictability, soft textures |
| Dual Sensory Loss | Use tactile signing, haptic devices, personal guides |
| Olfactory/Gustatory | Remove strong odors, explain food/taste differences |
| Digital Accessibility | Add captions, use alt text, provide keyboard access |
Communication Techniques and Augmentative Tools
Sometimes traditional speech isn’t enough. Augmentative and alternative communication (AAC) tools open up new options. These range from communication boards and picture cards to electronic speech-generating devices.
Sign language, tactile signing, and finger spelling are vital for many with hearing or dual sensory loss. Pictograms and color-coded charts help people with cognitive or processing barriers. Practicing patience, repeating or rephrasing information, and checking for understanding makes conversations smoother.
Staff training in AAC and inclusive communication methods can raise awareness and boost comfort levels for everyone involved.
Legal Rights
Do you know your rights when it comes to sensory accessibility? Laws in many countries guarantee access to information, education, and public life. If you or someone you know faces barriers, you can request reasonable accommodations from employers, schools, and service providers.
Examples of accommodations include:
- Captioned videos in meetings or classrooms
- Braille or large print on public documents
- Sign language interpreters for events
- Priority seating or tactile maps in transit systems
If you ever face resistance, organizations like the Disability Rights Education & Defense Fund (DREDF) can provide support and guidance.
Building Truly Inclusive Spaces
Lasting change happens when everyone works together. Listening to the experiences of people with sensory needs is the most valuable way to improve accessibility. Encouraging open communication, reviewing policies, and learning from feedback creates more welcoming environments.
Workplaces, schools, and community centers benefit from a culture of inclusion. Simple steps—like adding quiet rooms, captioning videos, or offering accessible events—pay off for everyone. Universal design not only supports those with sensory barriers but also makes spaces better for all.
If you’re looking to create a more accessible world, start small. Ask questions, educate yourself, and make adjustments where you can. Every change, no matter how minor it seems, brings us closer to truly barrier-free communication.
Conclusion
Sensory barriers to communication can make everyday life more challenging, but they don’t have to limit participation or connection. Through thoughtful design, technology, and community support, everyone can contribute to breaking down obstacles. Knowing your rights, using available tools, and sharing experiences makes a difference for yourself and others.
Want more ideas on supporting accessibility? Explore our resources or join the conversation in the comments.



